Condition | Brief Explanation | Treatment |
|---|
| Acute Hypothermia | Where the body's internal temperature falls below 35°C which disrupts regular cell function and homeostasis.
Symptoms: Rigors (shivering), slow and shallow breathing, confusion, loss of consciousness (coma), death. | Remove cold or wet clothing and wrap in foil blankets to conserve body heat (don't apply direct heat as can damage skin integrity). If unconscious, monitor breathing, warm intravenous fluids may be required. |
Acute Radiation Syndrome (Radiation Poisoning) | Caused by exposure to harmful radiation (particularly low wave-length EM radiation) which damages Cell DNA.
Symptoms: Nausea, vomiting, diarrhea, confusion, hair loss, internal bleeding, skin damage. | Decontamination (removal of irradiated items such as clothes and washing), Administration of Potassium Iodide. |
Anaphylaxis | An exaggerated immune response to an allergy, can result in closing of the airway (from inflammation) which can be stop breathing.
Symptoms: Chest tightness, problems breathing, vomiting, abdominal pain. | Adrenaline (for controlling initial inflammation) and IV fluids. |
Asthma (Flareup) | A chronic condition that causes overproduction of phlegm (secretions) which cause airway blockage, often brought on by exercise.
Symptoms: Breathlessness, coughing, bringing up lots of secretions. | Medication known as "Bronchodillators" that open up the airway. |
Cardiac Arrest | The heart stops beating, so organs are starved of oxygen and start to die.
Symptoms: No pulse, unresponsive. | Cardiopulmonary resuscitation (CPR) followed by defibrillation and oxygen therapy. |
Cardiovascular Accident (Stroke) | A blockage or damage to a blood vessel which has caused a lack of oxygen to reach the brain, causing damage. Three main types: Ischemic, blockage to a blood vessle caused by a blood clot. Hemorrhagic, blood vessle has blown (usually an aneurysm) causing a brain bleed, or TIA (transient Ischemic attack) where a clot has blocked a vessel but been dislodged in less than 24 hours.
Symptoms: Remember BEFAST - Balance (Can the person remain standing up straight), Eyes (Is there new blindness or blurred vision in one eye or double vision), Face (Is there a facial droop on one side?), Speech (Can the person produce clear coherent sentences or understand you?) Time (A stroke can cause permanent disability in minutes) | IT IS IMPORTANT TO FIRST DIAGNOSE WHAT TYPE OF STROKE AS TREATMENT FOR THE WRONG TYPE CAN CAUSE FURTHER DAMAGE.
For Ischemic stroke - CT Scan to rule out Hemorrhagic stroke, administer heparin (or any other anticoagulant medication) then D-Dimer to confirm clot, proceed to administer thrombolytic treatment.
For Hemorrhagic stroke - CT Scan to confirm and measure extend of brain bleed, if blood is significant surgery may be required to stop swelling (which can cause brain stem death). Administer Anti-Coagulant reversal agent to encourage clotting. |
Choking | A foreign object (usually food) has blocked the oesophagus and the patient can't breath.
Symptoms: Clutching at throat, gagging, pale appearance. | Back slaps and abdominal thrusts, oesophageal suctioning if prolonged. |
Chronic Obstructive Pulmonary Disease (Flareup) | A condition that causes more ineffective breathing overtime, usually caused by smoking damage to lungs. Flareups in struggling to breath are usually caused by chest infections.
Symptoms: Rapid and shallow breathing, producing lots of secretions, fatigue, blood in cough, wheezing. | Medication known as "Bronchodillators" that open up the airway, oxygen is also given. |
Heart Attack | A blockage, usually caused by a blood clot, has traveled to the heart valve and stopped blood flow causing poor circulation.
Symptoms: Sharp pain in chest and left arm, chest tightness, low or high blood presure, signs of acute heart failure. | Initially blood thinners such as Aspirin, then either breaking down the clot (thrombolysis) or surgery to implant a stent. |
Hypoglycemia | Low blood sugar, often a complication of Diabetes. Causes cells to not receive required energy. Considered a medical emergency.
Symptoms: Sweating, heart palpitations, fatigue, confusion and eventually coma. | Administered glucose (sugar) by either eating or IV (depending on if patient is comatose). |
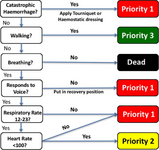
Major Trauma | Significant structural damage to the body including extensive blood loss, broken bones, burns and injured organs.
Symptoms: Catastrophic Hemorrhage, one or more organs shut down. | Major, often complex surgery with IV bloods, fluids and medications given. Escalation to intensive care. |
Pulmonary Embolism | A blood clot in the lungs blocking (occluding) effective respiration (gas exchange of oxygen and carbon dioxide). 'PE' can cause lung damage or the clot can travel towards the heart and cause a heart attack.
Symptoms: Chest pain, coughing blood, dizziness or fainting. | Initially blood thinners such as Aspirin, then either breaking down the clot (thrombolysis) or surgery to implant a stent. |
Seizure | A surge of electrical activity in the brain causing temporary dysfunction, there are different types of seizure ranging from focal (area specific, such as shouting or absence seizures) to generalized (full body, most commonly tonic-clonic seizures that result in convulsions). Any seizure lasting over 5 minutes is considered an emergency requiring treatment. Epilepsy is the most common seizure disorder.
Symptoms: Dependent on seizure, but can include; vacant expression, unresponsiveness, convulsions, loud vocalizations (shouting) and anxiety. | Any seizure lasting more than 5 minutes is considered "Status Epilipticus" and considered an emergency. Benzodiazepines are used to control symptoms, underlying causes must then be treated (e.g., pain). |
Sepsis | Known as septicemia (blood infection), the body's immune system over-reaction to an infection causing a decrease in blood pressure and high pulse, low temperature and oxygen desaturation (low oxygen levels in the blood). Sepsis left untreated results in septic shock which causes organ failure, each hour sepsis is left untreated, fatality risk increases by 10%.
Symptoms: Low blood pressure (due to low blood volume), fast pulse, high or low temperature and decreasing oxygen levels, pale mottled-skin appearance, low frequency of urination, feeling of going to die, confusion. | See "SEPSIS 6"; fluids, antibiotics and oxygen therapy. |
Shock (Cardiogenic, hypovolemic, obstructive and distributive) | Reduced perfusion (oxygen exchange) between cells due to changes in blood distribution. Four main types (distributive - including septic shock, cardiogenic, hypovolemic, obstructive).
Symptoms: Pale or cyanosis (blue skin), fast pulse, shallow breathing, restlessness or unresponsive.
For more information about shock: Click Here | Treating the underlying cause, vasoconstriction that tighten blood vessels, blood and fluids. |
Traumatic and Non-Traumatic Brain Injury | A traumatic brain injury includes physical impaction of the head causing structural damage to the brain. non-traumatic brain injury is internal factors including hypoxia (oxygen starvation), stroke or overdose.
Symptoms: Loss of consciousness, seizures, cognitive impairment (issues with thinking, planning and understanding), neurological impairment (nerves, muscle control etc). | Treating the underlying cause (surgical repair, removing blood clot etc.) Brain injuries often result in long-term, irreparable damage to nerves resulting in cognitive impairment, epilepsy, muscle weakness and dysphasia (trouble with speaking). |
Overdose | Overdose is a type of poisoning and can vary greatly on affects, but essentially is the introduction of substances that are either toxic or consumed in toxic amounts. In this we are including alcohol as a substance.
Symptoms: Dependent on substance but may include; diarrhea and vomiting, seizures, liver failure, high temperature, respiratory depression, cardiac arrest. | Usually involves either removing or flushing out the toxin with IV fluids, activated charcoal can be used if overdose was taken recently. |